Stem Cell Therapy: Where Should You Go for the Best Treatment?
Stem cell therapy is a type of regenerative medicine that uses stem cells as a treatment for certain conditions. Mexico, Colombia and other countries start
Stem cell therapy is a type of regenerative medicine that uses stem cells as a treatment for certain conditions. Mexico, Colombia and other countries start

For more than two decades, Dr. Riordan’s Stem Cell Institute has been at the forefront of regenerative medicine, pioneering innovative stem cell therapies that
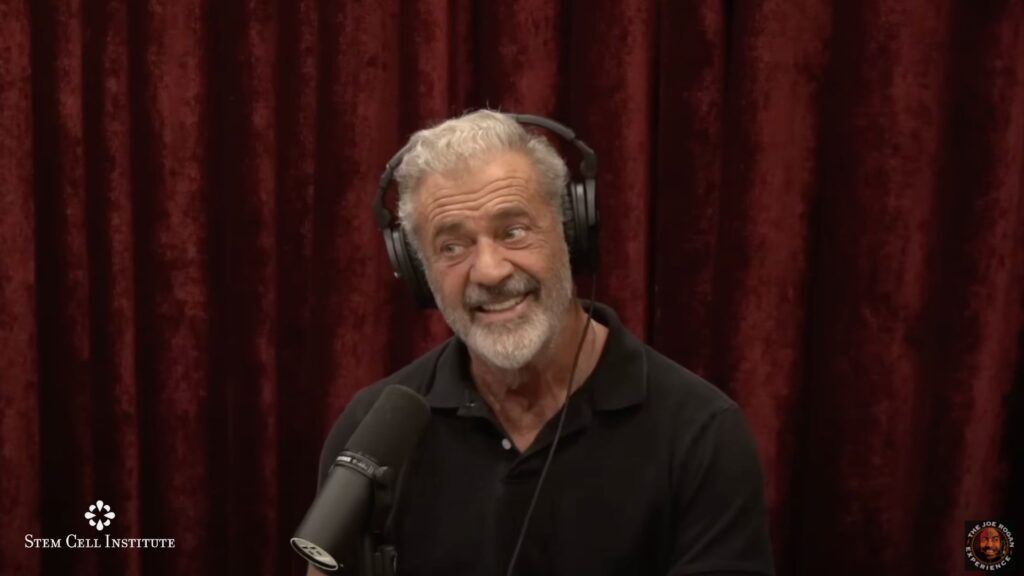
Mel Gibson is an award-winning actor, director, and producer. In a recent interview on The Joe Rogan Experience, Gibson shared his personal experience with stem

Stem cell-related supplements are dietary products marketed as support for the body’s natural regenerative processes. Often sold in stores or online like common vitamins, these
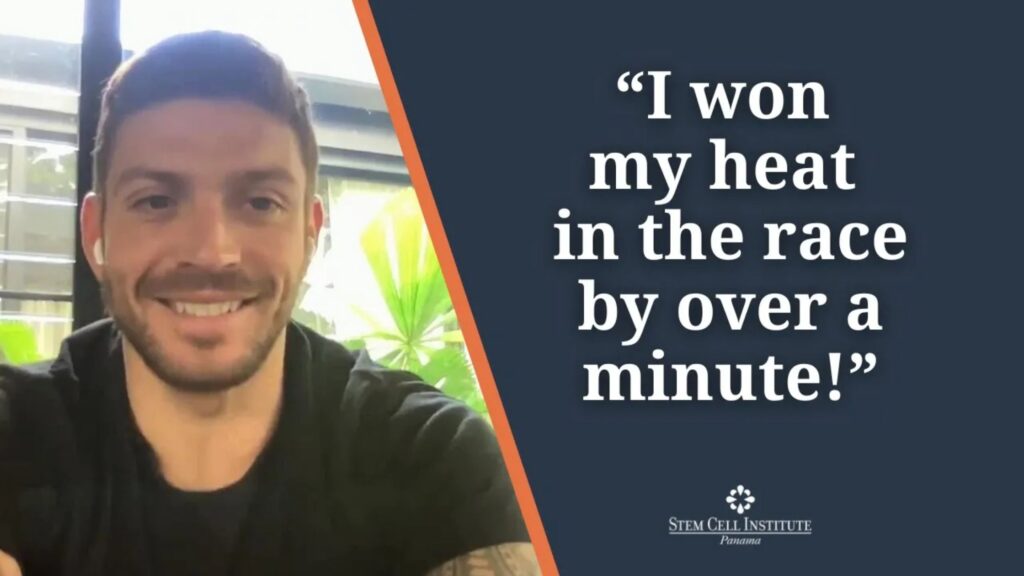
Luke Zocchi is a personal trainer who gained fame as Chris Hemsworth’s long-time fitness coach. Their connection dates to childhood, as they attended primary and

With public endorsements from celebrities such as Tony Robbins and John Cleese, stem cell therapy to fight the normal aches and pains of aging has
Toll Free:
1-800-980-STEM (7836)
Outside or Inside US Call:
1-954-358-3382
Toll Free Fax (US Only):
1-866-755-3951
From Outside US Fax:
1-775-887-1194
Copyright 2025, Stem Cell Insitute Panama. All rights reserved.