It gave me hope that there’s a light at the end of the tunnel.
At Stem Cell Institute we offer patients an opportunity for an independent and healthier life.
It gave me hope that there’s a light at the end of the tunnel.
At Stem Cell Institute we offer patients an opportunity for an independent and healthier life.
You deserve the world’s leading stem cell therapy and research center.
For over 15 years Stem Cell Institute has provided Advanced Adult Stem Cell Therapies that have been thoroughly researched and tested.






OUR PROCESS
Begin your journey to a healthy and independent life.
Here’s how to do it.
1. Apply Today
Upon approval of your application, our doctors will craft a unique treatment plan based on your specific needs.
2. Receive Treatment
Our patient concierge will help you arrange an exceptional stay in Panama City to receive your treatment.
3. Follow Up
After treatment, our team will follow up with you at regular intervals to monitor progress and provide support.
CONDITIONS
Has your life been impacted by chronic illness, injury, or neurodiversity?
Our medicine is founded on clinical use of stem cells.
In order to incorporate the most recent advancements into patient care, we routinely interact with colleagues in the USA and internationally, many of whom are using stem cells in clinical trials.

Stem cells worked wonders for my shoulder after struggling with excruciating pain.
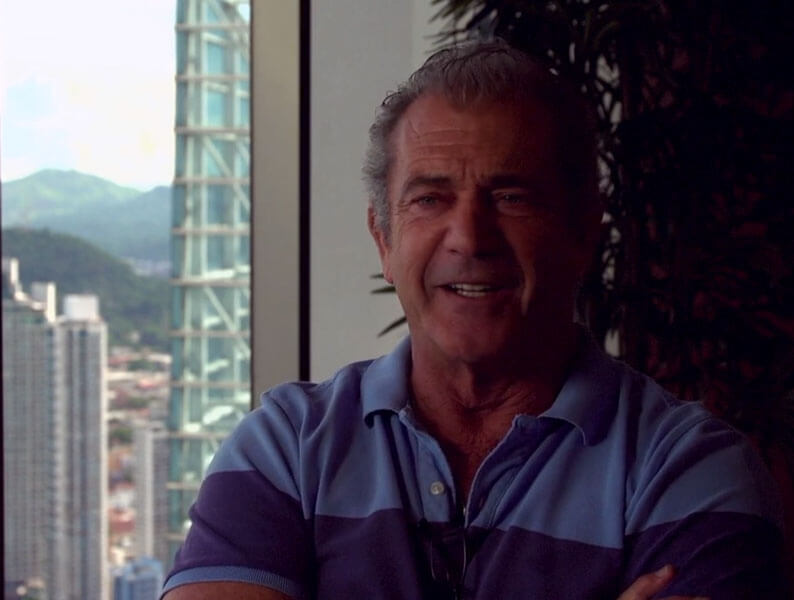
It was like he got a new lease on life.

I sent my mom down there twice and it did wonders for her.
FREQUENTLY ASKED QUESTIONS

You probably have questions. We’re here to help.
If you wish to send medical records to us, do not send them to the address on this page. Special instructions are required to ensure that records arrive to our clinic in Panama. Please contact us for more information.
To start your free evaluation, please complete our online Patient Application. If you still have questions, please feel free to contact us today!
Golden Cells™ are highly effective cells from six particular cell lines. After a retrospective analysis of our most successful procedures, we discovered that these particular cells were almost always present. We have developed the technology and procedures to identify, isolate, and grow these Golden Cells™ for adminstering to our patients.
Generally speaking, aside from the initial pain at the injection site, the patient will not experience any discomfort. Less than 10% of (mostly lumbar puncture) patients have developed a minor fever, headache, nausea or vomiting. However, these side effects have never lasted more than three days and usually resolve within 24 hours. No long term negative side effects have been reported.
We receive cord donations from healthy women in Panama following normal births. Our donors sign a consent form, fill out a detailed questionnaire, and give a blood sample. The mothers’ blood undergoes extensive testing for HIV, STD’s, hepatitis, etc.
Adult stem cells are not encompassed by the controversy surrounding fetal and embryonic stem cells. Both the Catholic Church and the Southern Baptist Church have issued papers which actually encourage research and the use of adult stem cells in the treatment of human disease as an ethically acceptable alternative to the use fetal and embryonic stem cells.
OUR FOUNDER
Neil H. Riordan
PA, PhD
Our science originates from an American biotechnology company founded by Neil Riordan, PhD who together with leading Universities has published numerous papers in peer reviewed medical journals and has 17 families of patent applications.


Read Dr. Riordan’s book “Stem Cell Therapy: A Rising Tide”
“Neil takes readers on a riveting journey through the past, present, and future of stem cell therapy. His well-researched, educational, and entertaining book could change your life. I highly recommend it.”
– Tony Robbins, NY Times #1 Bestselling Author










